
Cannabis-Based Medicine For Patients Living With Multiple Sclerosis
What Is Multiple Sclerosis (MS)?
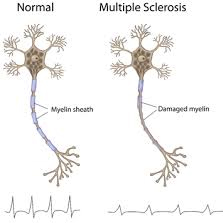
Multiple Sclerosis is an autoimmune, inflammatory condition which is caused by an attack from the body’s immune system on the myelin sheath that surrounds nerve cells in the central nervous system (CNS). The myelin sheath provides insulation to these cells to allow for fast conduction of signals throughout the body; destruction slows the speed of signals from the CNS to the body’s peripheral nervous system (PNS). This condition can also lead to destruction of the nerves themselves, which is irreversible.
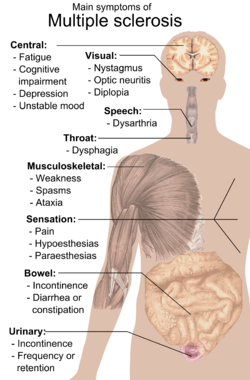 Due to the fact that the CNS is the “command center” for the body, MS can cause problems in numerous body systems. Multiple Sclerosis (and the current treatments available for its treatment) can cause bladder infection and dysfunction, bowel dysfunction, depression, fatigue, itching, emotional changes, pain, sexual problems, tremors, dizziness and vertigo, gait (walking) difficulties, sleep disturbance, and more.
Due to the fact that the CNS is the “command center” for the body, MS can cause problems in numerous body systems. Multiple Sclerosis (and the current treatments available for its treatment) can cause bladder infection and dysfunction, bowel dysfunction, depression, fatigue, itching, emotional changes, pain, sexual problems, tremors, dizziness and vertigo, gait (walking) difficulties, sleep disturbance, and more.
One major symptom of Multiple Sclerosis is referred to as spasticity. It can cause overactive reflexes, involuntary movements, difficulty with care and hygiene, abnormal posture, contractures, pain, bone and joint deformities, and more. Needless to say, Multiple Sclerosis causes a severely decreased quality of life for patients. There is currently no cure for Multiple Sclerosis, which is why research for new treatments for symptom relief and disease progression is imperative.
Results From The Largest Study On Cannabis, MS To Date
One of the largest studies gauging the effect of medical cannabis on patients with Multiple Sclerosis was one of 630 participants conducted by Zajicek et al. in 2003 at 33 centers. Results showed that participants who used whole-plant cannabis-based medicine (CBM) extracts did not experience an improvement in objective measurements of spasticity measured by the Ashworth scale – a tool used to assess objective measures of spasticity, including tone, resistance, and rigidity in body extremities.
“Patients in the CBM extract or ∆-9-tetrahydrocannabinol (THC) CBM groups reported improvements in “pain, sleep quality, spasms, and spasticity.” – Zajicek et al.
However, in self-reports, patients in the CBM extract or ∆-9-tetrahydrocannabinol (THC) CBM groups reported improvements in “pain, sleep quality, spasms, and spasticity,… though no effect was noted with respect to irritability, depression, tiredness, tremor or energy.”
In comparing the lack of efficacy for spasticity as measured by the Ashworth Scale to other treatment options available for Multiple Sclerosis, Zajicek et al. importantly note the following:
“When assessing our results, it should be acknowledged that the degree of evidence for many of the commonly used drugs to combat [Multiple Sclerosis] symptoms is weak… One study [of a commonly used medication for Multiple Sclerosis] noted a difference in Ashworth scores comparing active treatment with placebo, whereas the other showed no effect. Neither of these studies detailed any difference in walking times [, another measure of disability caused by Multiple Sclerosis], and even when a significant effect was obtained in the Ashworth score, there was no different in pain measures or sleep quality on active medication.”
In contrast, medical cannabis did show efficacy in improvement of pain and sleep quality. Additionally and importantly, at the 12-month follow-up, “muscle spasticity measured by the Ashworth scale was significantly improved in the THC-treated [CBM] group. The Rivermead Mobility Index [a test of functional mobility] was also improved, indicative of reduced disability.”
Using Objective Reporting Measures When Treating MS
So if medical cannabis did not show immediate efficacy on the Ashworth Scale in such as large study, this treatment option is not effective a good treatment option for Multiple Sclerosis, right? The answer to this question is a strong and resounding “no”; comprehension of the reasoning for this requires a basic understanding of tools used in research.
Validity tests (those that gauge whether or not a tool is accurate/whether it measures what it is designed to measure) and reliability tests (those that gauge the ability of a tool to produce the same results when administered multiple times in the same conditions) are performed on tools like the Ashworth Scale, in order to help us to understand their real-world or clinical utility.
 Zajicek et al. noted in their large 2003 study, “The limitations of the Ashworth scale in measuring the highly complex symptom of spasticity are well known, and there is a need to develop new patient-oriented scales to enable measurement of what matters to them.”
Zajicek et al. noted in their large 2003 study, “The limitations of the Ashworth scale in measuring the highly complex symptom of spasticity are well known, and there is a need to develop new patient-oriented scales to enable measurement of what matters to them.”
Due to the fact that the Ashworth scale is not a fully valid measure of spasticity, performance on it should not be used in the assessment of treatment efficacy. Whether medical cannabis is able to produce significant change in the Ashworth Scale therefore does not properly measure the efficacy of medical cannabis on spasticity.
Additionally, there are many other symptoms experienced by patients with Multiple Sclerosis than just spasticity (such as pain, weakness, etc.), and treatment efficacy should not be gauged solely on changes in that one symptom.
According to Vaney et al., “…it must be questioned if disturbance of muscle tone by strong anti-spastic agents is in every case clinically meaningful as disability in Multiple Sclerosis patients seems more clearly related to weakness than to spasticity.”
In a study using CBM capsules with 2.5 mg THC and 0.9 mg cannabidiol (CBD), these same researchers found that “there were no statistically significant differences associated with active treatment [i.e. medical cannabis] compared to placebo, but trends in favor of active treatment were seen for spasm frequency, mobility and getting to sleep.”
“Treatment with smoked cannabis resulted in a significant reduction in patient [modified Ashworth Scale] scores.” – Corey-Bloom et al.
Further, studies have shown improvement in objective ratings of spasticity. Using the modified Ashworth Scale (MAS), a study conducted in 2012 by Corey-Bloom et al. found that “treatment with smoked cannabis resulted in a significant reduction in patient scores… In addition, treatment reduced pain scores on a visual analogue scale [a self-report measure].”
No difference was found between medical cannabis and placebo groups on a timed walk test. However, scores on a test of cognitive function showed lower scores for participants on active treatment compared to the placebo group.
Using Subjective Reporting Measures When Treating MS
So what tools should researchers utilize to measure improvements in spasticity symptoms for patients with Multiple Sclerosis? In a 2010 meta-analysis of the efficacy of oromucosal CBM and MS, Wade et al. stated the following:
“The 0-10 Numerical Rating Scale is recommended as a preferred outcome measure in the assessment of interventions in chronic pain, but has not been widely used in studies of anti-spasticity medications. It has the benefit of allowing the patient to express their own daily experience of spasticity and has recently been validated… it is a suitable assessment tool and possibly an alternative to the Ashworth Scale which several research groups have criticized.”
 The researchers “found that global impression of change (GIC) was significantly improved for patients on active treatment [i.e. medical cannabis]. Participants on active treatments were significantly less likely to experience spasticity compared to placebo participants, based on self-reports of Visual Analogue Scale and Numerical Rating Scale.”
The researchers “found that global impression of change (GIC) was significantly improved for patients on active treatment [i.e. medical cannabis]. Participants on active treatments were significantly less likely to experience spasticity compared to placebo participants, based on self-reports of Visual Analogue Scale and Numerical Rating Scale.”
In scientific study, self-report measures are considered unreliable because humans possess bias by nature, often unintentionally. Scientists understandably desire facts and not opinions, which is the reason why objective measures and double-blinding are used as elements of the gold-standard for determining treatment efficacy.
However, a study by Collin et al. (2007), which found efficacy of CBM using self-report measures addresses this issue in relation to CBM treatment and Multiple Sclerosis. The researchers mention in the “Discussion” section of their study that although their work was criticized for the utilization of a self-report measure, it may actually be superior to observer-rated measures.
One reason for this is the lack of “clinical relevance” that objective measurements provide; when “real world” patients with spasticity go to see their physician, the physician often merely asks either the patient or their caregiver how the patient has been feeling about their spasticity. Very rarely are objective measures like the Ashworth Scale utilized.
Additionally, utilization of the 11-point Numeric Rating Scale is meant to provide a broader view of the patient’s experience of their spasticity. It does so by measuring spasticity over 24 hours, not at only one point in time, thereby gaining a better idea of the patient’s quality of life.
As noted by Collin et al., “there is increasing acceptance that a patient reported outcome measure is appropriate for spasticity.” The NRS is frequently used for pain assessment in the clinic, with at least a 30% reduction in pain after treatment signifying that the treatment provided a “clinically meaningful reduction in pain”.
While it is unclear whether or not the same gauge is appropriate to assess whether or not the NRS can be used to accurately measure spasticity with reliabilty, 40% of the original CBM group in this study experienced a >30% improvement in their spasticity. This improvement was found in addition to those already provided by the participants’ prescribed medications for anti-spasticity, which they were required to continue throughout the trial.
The researchers note, “Small improvements in the patients[’] experience may lead to large changes in quality of life… The ideal objective measure of spasticity does not exist. Using the NRS [for spasticity research] as in pain research appears to be a reasonable compromise.”
Evidence For Efficacy Of Cannabis-Based Medicine On MS
Multiple studies have shown the benefits of medical cannabis for patients with Multiple Sclerosis experiencing a wide range of symptoms. Novotna et al. (2011) conducted a Phase III placebo-controlled trial on cannabis-based medicine (CBM) as an add-on therapy for MS symptoms. The CBM add-on produced a “highly significant” difference in the Numeric Rating Scale, as well as improvements in self-reports of spasm frequency, sleep disturbance, and perspective of the caregiver and clinical regarding global impression of change for the patient.
In 2007, Collin et al. conducted a study on the effects of CBM on patients with Multiple Sclerosis and found that oromucosal CBM significantly improved daily subject-recorded Numerical Rating Scale of spasticity. However, there was no significant difference between placebo and active treatment [i.e. medical cannabis] on Ashworth Score and the Motricity Index [an objective measure of muscle power]. 57% of participants on active treatment vs. 48% of control participants experienced an improved global impression of change of symptoms.
 Numerous studies have also shown the efficacy of medical cannabis in treating neuropathic pain, which is the most common pain type experienced by patients with Multiple Sclerosis. These include “A Randomized, Placebo-Controlled, Crossover Trial of Cannabis Cigarettes in Neuropathic Pain” by Wilsey et al. (2008) and “Smoked cannabis for chronic neuropathic pain: a randomized controlled trial” by Ware et al. (2010), which also showed improvements in ability to fall asleep, improved quality of sleep, and well-tolerated and minimal adverse events.
Numerous studies have also shown the efficacy of medical cannabis in treating neuropathic pain, which is the most common pain type experienced by patients with Multiple Sclerosis. These include “A Randomized, Placebo-Controlled, Crossover Trial of Cannabis Cigarettes in Neuropathic Pain” by Wilsey et al. (2008) and “Smoked cannabis for chronic neuropathic pain: a randomized controlled trial” by Ware et al. (2010), which also showed improvements in ability to fall asleep, improved quality of sleep, and well-tolerated and minimal adverse events.
Additionally, “A Preliminary Controlled Study to Determine Whether Whole-Plant Cannabis Extracts Can Improve Intractable Neurogenic Symptoms” by Wade et al. (2003), which used oromucosal CBM, found improvements in pain, impaired bladder control, muscle spasms and spasticity with medical cannabis treatment.
CBM As Treatment Of The Disease, Not Just The Symptoms
There is some evidence that suggests that medical cannabis may be useful beyond symptom control for patients with Multiple Sclerosis, and may be able to act as direct treatment of the disease.
“Preclinical evidence has emerged supporting th[e] hypothes[is]… that…activation of CB2 receptors expressed by T cells within the central nervous system will decrease inflammation in MS and possibly also slow progression of the disease.” – Pertwee et al.
A study by Pertwee et al. (2007) conducted a review on cannabinoids and their effect on Multiple Sclerosis, found that there is evidence to suggest that cannabinoids may work not only as a treatment for MS symptoms, but also the direct treatment of the disease.
This is believed to occur through activation of cannabinoid receptors which “may suppress some of the pathological changes that give rise to these signs and symptoms”.
The researchers note, “signs and symptoms of this disease can be ameliorated by cannabinoid receptor agonists at doses that do not provoke unacceptably severe adverse events. Preclinical evidence has emerged supporting th[e] hypothes[is]… that…activation of CB2 receptors expressed by T cells within the central nervous system will decrease inflammation in Multiple Sclerosis and possibly also slow progression of the disease.
Cognitive Effects Of Cannabis On People With MS
To date, some of the evidence that suggests that medical cannabis is a harmful treatment option for patients with Multiple Sclerosis points to the fact that on cognitive tests, MS patients who use medical cannabis may perform worse in comparison to Multiple Sclerosis patients who did not use medical cannabis.
Given that the disease itself can cause cognitive declines, these results represent an understandable concern. However, when discussing conditions like Multiple Sclerosis with debilitating symptoms, maintenance of optimal cognition is not the most important issue.
A patient using medical cannabis with decreased pain, greater ease in sleeping, decreased self-reports of spasticity, and/or an increase in global perception of their health, is a medical success.
CBM Is A Safe, Effective Treatment Option For Patients With MS
Given its low risk of negative side effects and low risk of dependence, CBM may be an effective treatment option to be used in conjunction with other efficacious treatments for patients with both typical and intractable Multiple Sclerosis symptoms. However, medical cannabis is not an optimal treatment option for everyone.
“It would be beneficial for patients with multiple sclerosis to have safe, legal access to various forms of medical cannabis, with use authorized and monitored by their healthcare provider.”
To gain a better understanding of the CBM and its effects on Multiple Sclerosis, more research needs to be conducted using proper tools in order to assess its effects.
With that said, increased research for any medication is always warranted – even for those that have been legal and commonly used for decades. Thus, this is not a strong enough reason to maintain prohibition on medical cannabis for patients with Multiple Sclerosis.
The evidenced overall safety of medical cannabis in various forms, along with its shown efficacy for various symptoms of Multiple Sclerosis, seems to support its use for patients who are suffering. This is especially true of those with intractable symptoms which cannot be ameliorated by other therapies.
In turn, it would be beneficial for patients with multiple sclerosis to have safe, legal access to various forms of medical cannabis, with use authorized and monitored by their healthcare provider.
For information on reasonable expectations and safety in considering whole-plant medical cannabis use, as well as how you can advocate to move cannabis out of the Schedule I controlled substance classification in order to increase research on phytocannabinoids in the United States, click here.