
Study: Cannabis Offers Possible Treatment for High Grade Gliomas
A study published in November 2014 in Molecular Cancer Therapeutics and conducted at St. George’s University of London’s Department of Oncology has found that the use of cannabinoids, specifically delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD), may be useful in treating high-grade gliomas, potentially slowing the disease’s progression.
What Are High Grade Gliomas?
Gliomas are a type of advanced brain cancer that are fast-growing, aggressive, and difficult to treat. Gliomas occur in the brain and spinal cord and result from the excessive proliferation of abnormal neuroglia, cells of the nervous system that are not directly involved in signaling (as opposed to neurons). Usually, neuroglia work in important, supportive roles to ensure that neurons are communicating properly and efficiently, and there are 3 neuroglia for every 1 neuron in the body. Types of gliomas include astrocytomas (the most frequent type), ependymomas (the most common glioma in children), and oligodendrogliomas.
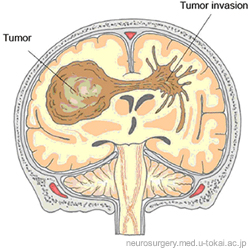 There are benign gliomas (which do not invade brain tissue and can be removed if in certain locations, only producing symptoms if they begin to compress important surrounding structures) and malignant gliomas (which do invade brain tissue and have a worse prognosis, or an increased likelihood of shortened survival). So, while not all gliomas are malignant, 80% of malignant brain tumors are gliomas. In the United Kingdom, 1-year survival at diagnosis of a high grade glioma is 36%, and 5-year survival is 10%.
There are benign gliomas (which do not invade brain tissue and can be removed if in certain locations, only producing symptoms if they begin to compress important surrounding structures) and malignant gliomas (which do invade brain tissue and have a worse prognosis, or an increased likelihood of shortened survival). So, while not all gliomas are malignant, 80% of malignant brain tumors are gliomas. In the United Kingdom, 1-year survival at diagnosis of a high grade glioma is 36%, and 5-year survival is 10%.
For glioblastoma multiforme, a particularly aggressive high grade glioma, the majority of patients diagnosed pass away within 1 year, and 5-year survival is only 6%. While surgery, radiation, and chemotherapy can be used in attempts to treat high grade gliomas, there are very few to no effective treatment options that increase patient survival, and finding ways to extend the lives of patients is desperately needed.
Cannabinoids as Anticancer Agents
This is not the first time that a study has shown that cannabinoids may be useful as anticancer agents. According to the authors of the study, “Numerous reports highlighting potent activity in vitro [i.e. cells studied outside of the body] and in in vivo [i.e. cells studied inside the body] models have established it as a potential anticancer therapeutic agent in a number of cancer types through processes such as:
- induction of apoptosis [i.e. programmed cell death]…
- autophagy [i.e. “self-eating”/”self-destruction”] via engagement of the mitogen-activated protein kinase [i.e. an enzyme activated by an agent which induces mitosis, the process by which cells increase in number, which is how cancerous tumors form] and the endoplasmic reticulum [i.e. an organelle, or part of the cell, involved in protein and lipid synthesis] stress-related pathways…
- antiangiogeni[sis] [i.e. preventing formation of blood vessels, which cancerous growths need to survive]…
- anti-inflammatory [actions]
- anti-migratory[actions]
 While the authors note that the psychoactive nature of THC has increased controversy in consideration of cancer treatment with its use,” a pilot trial of its therapeutic use in patients with glioblastoma multiforme (GBM), an advanced type of glioma, showed feasibility without any overt psychoactive effects.”
While the authors note that the psychoactive nature of THC has increased controversy in consideration of cancer treatment with its use,” a pilot trial of its therapeutic use in patients with glioblastoma multiforme (GBM), an advanced type of glioma, showed feasibility without any overt psychoactive effects.”
Additionally, CBD seems to work through similar mechanisms as THC in terms of anti-tumor effects, except it may not exert effects through receptor activation as frequently as THC, and it does not cause psychoactive effects. Further, THC demonstrates analgesic, anti-emetic, and anti-inflammatory properties, whereas CBD possesses anti-psychotic, anti-seizure, and anti-anxiety properties. Together, these cannabinoids (and many more) work together to create an entourage effect that is much more powerful than any single cannabinoid.
Results of the Current Cannabinoid Study
in-Vitro
For the in-vitro portion of the study, the researchers evaluated the effects of THC and CBD on GBM and glioblastoma astrocytoma cells.
Cannabinoids Alone
- They found that use of CBD and THC in pure form (>96% purity) and in their whole-plant forms (60% to 72% of each cannabinoid) decreased the number of high grade glioma cells in a dose-dependent manner.
- Analysis of the cells showed that there were no changes made to cell DNA, which points to the mechanism of action being one of cytostasis (i.e. prevention of cell growth and proliferation). The effect was greater for GBM cells than for glioblastoma astrocytoma cells.
- Rather than causing apoptosis, the cannabinoids seemed to inhibit cell growth and proliferation via autophagy.
- Additionally, it was found that CBD was more effective in inhibiting cell growth in its pure form, while THC was more effective in its whole-plant form.
- The combination of CBD and THC seemed to have even greater effects (for glioblastoma astrocytoma more than for glioblastoma multiforme), although these results were not statistically significant (i.e. it is fairly likely that this association occurred by chance).
- CBD and THC appeared to control cytostasis through mechanisms such as modification of phosphorylation patterns in cell signaling pathways which lead to increased cell growth and proliferation, most significantly through MAPK pathways after use of pure CBD or THC for 4 hours, but also through ERK pathways for glioblastoma multiforme cells (and glioblastoma astrocytoma cells, when CBD was used alone), with potential for modulation through the AKT pathway. At high doses, cannabinoids decreased AKT and and ERK pathway activation, and even more significantly when radiation was used in conjunction.
Cannabinoids Plus Radiation
- When cells were pre-treated for 4 hours prior to radiation treatment with pure CBD, pure THC, or a combination of pure CBD and THC, it was found that the combination reduced the number of high grade glioma cells after radiation (i.e. incubation in the combination of cannabinoids made the cells more sensitive to destruction by radiation). Additionally, 5 hours post-radiation, high grade glioma cells that had been treated with cannabinoids had more DNA damage than cells that had been treated with radiation alone (this is a positive result, given that the point of radiation treatment is to damage the DNA of malignant cells in order to cause programmed cell death).
- The only time that induction of apoptosis as the antitumor/anticancer mechanism of action was examined was in use of radiation combined with high doses of cannabinoids.
in-Vivo Mouse Model
For the in-vivo portion of the study, the researchers evaluated the effects of THC and CBD on C57BL/6 mice with transplanted GL261 glioma tumors. 80% of mice who received transplants developed tumors, and the researchers found that radiation alone had no effect on glioma growth, while combined THC and CBD inhibited progression, and combined THC, CBD, and radiation inhibited progression the most.
When the brains of the mice were examined after death, it was found that the groups that had been treated with cannabinoids had cancerous growths that were denser than in mice who had not been treated with cannabinoids, suggesting inhibited progression. Additionally, the “vascularization marker” CD31 was reduced in mice who had been treated with cannabinoids (in order to grow and spread, tumors need a blood supply, and increased vascularization is usually a sign of more aggressive growths and a worse prognosis). TUNEL staining was also often increased in the brains of mice who had been treated with cannabinoids, signaling increased DNA fragmentation, especially in combination with radiation treatment (again, this is a positive sign for inhibition of growth/proliferation).
Conclusion
According to the researchers, “…[T]hese data add further support to the concept that cannabinoids both alone and in combination with each other, possess anticancer properties.” Given this exciting new evidence, in conjunction with the previously existing evidence supporting the potential application of cannabinoids as antitumor/anticancer agents, increased research on the use of cannabinoids in treatment of not only high grade gliomas, but also other types of cancerous growths, is warranted and needed as soon as possible.
For information on how you can advocate to move cannabis out of the Schedule I controlled substance classification in order to increase research in the United States, expectations, and safety in considering whole-plant medical cannabis use, click here.